You’ve been seeing the commercials, the news, the stories about stars, and stories about the everyman losing gobs of weight on GLP-1s like Mounjaro, Zepbound (which is a GIP/GLP-1), Ozempic, and Wegovy (GLP-1). Perhaps you have the important desire to improve your health and are considering the medications. Now you’re wondering if they are for you. Who do you ask about them? How do you talk to that provider? What if you are prescribed the medication? What role does your provider have during your GLP-1 experience? What if the person you ask tells you that you don’t need it or qualify for it? What if they tell you they don’t believe in them? Where do you go from there?
Who Do You Ask for the GLP-1s?

I use the term “Doctor” throughout this post, but know that not all Primary Care Providers (PCP) are physicians. It’s good to know this because you might have a Certified Nurse-Practitioner (CNP), a Certified Nurse Midwife (CNM), a Psychiatrist (who is an MD), a Dermatologist (an MD or CNP), a Plastic Surgeon (an MD), Physician Assistants (PA), an Osteopathic Doctor (DO), an Endocrinologist (a CNP or MD), a Clinical Nurse Specialist (CNS), and in certain states, a Naturopathic Doctor (ND), or a Functional Medicine Doctor (FMD), along with other providers might prescribe the meds for you. If unsure who can prescribe for you, Google “Who can prescribe weight loss drugs <insert city where you live>” The term “weight loss drugs” is a catchall for the GLP-1 medications, whether they are for weight loss or diabetes treatment.
Bringing Up the Topic of GLP-1s With Your Doctor

Some providers will be more amenable to prescribing GLP-1s than others, but it’s good to get different opinions even if the first person you try tells you no. Be sure to ask why and listen to what they have to say. Then, if you disagree or still want the medication, you move on to find a new provider.
So you’re sitting in the doctor’s office and you’ve either had a health exam or not, I encourage people to talk about serious topics with their clothes on. So either before the exam begins or is over is ideal. Most doctors are in a hurry, but you have a right to their time for your important questions. It’s always good to have a list of questions so you don’t forget anything.
Things you might say to get the discussion started:
- I’ve heard a lot about the new medications for diabetes/weight loss. What do you think of them?
- Have you ever prescribed the new weight loss medications? (If yes…) Who do you typically prescribe them for? (If no…) Do you not like them?
- I have a friend on Ozempic/Wegovy/Mounjaro/Zepbound and she loves it. What do you think?
- Do you think I might be qualified to take one of the new weight loss medications?
- I’m worried about my health because of my weight. Might those new medications be a good choice for me?
- I’ve been researching those new GLP-1 medications and wondering if you thought they might be helpful for me.
The way these questions are worded will not put the doctor on the defensive, but allows them to give you their honest opinions because you are asking in a curious way. If you act like you know nothing, they are able to teach you and practitioners love nothing else more than teaching. If you act like you know everything, you turn them off completely. Even if you have studied and researched and know a lot about the medications, asking questions of the provider really opens the door to good communication.
What If the Doctor Says No?

I encourage you to not try and convince the doctor to give you a prescription. It’s far better to move on and find someone else. Pushing is not the best way to positive communication with the person caring for you.
There are so many ways to be prescribed the medications now, including telehealth companies. I highly encourage finding one that has MDs or DOs on staff if not interviewing you personally. Don’t just go by word of mouth on the Internet, but research and find who is qualified and safe to be prescribing these meds.
What If Your Doctor Says Yes?

You are halfway there! The issue becomes whether your insurance, if you have it, will pay for it or not. Insurance companies are asking for a Pre-Authorization (PA) to get the prescription written. The provider has to send in a PA and you are in limbo until the PA is approved. This means the insurance company is the judge and jury of whether they think you are qualified to get the meds or not. If they say no, that is just the first try. The doctor might not have given enough information for them to make a determination yet. I have seen PAs sent in four times, with new information added each time, before being approved. Mind you, not all doctors are hip to the PA game and will only try once. I encourage an email to politely ask them to try again, please.
If you are finding brick walls around the PA, it would be great to call your insurance company and ask what exactly is missing from the PA. Then you can email the doctor and tell them, politely, that you talked to the insurance company and they told you <this or that> was missing and perhaps they could try again with that information?
It’s much easier for you to call the insurance company in the middle of the night. They are open 24 hours a day and you won’t have to wait forever on hold that way. You will typically not be rushed, either.
What Might Your Care Look Like While On
Health Gain and Weight Loss Medications?
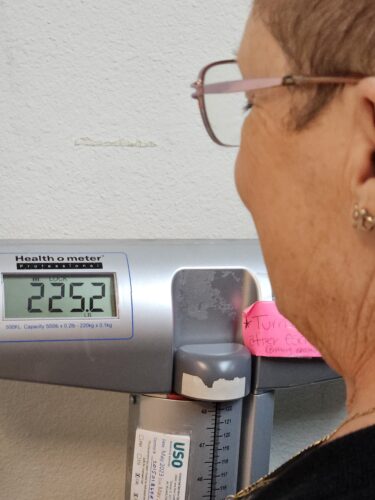
This topic is so variable it will be hard to generalize.
Some providers take a real hands-on approach and want to see you each month to give you your injection. This can get old for many people and they eventually ask to give themselves the shots. They are shown how, then practice giving one in front of the doctor or nurse, and sent off on their own for a month or three unless they need to be seen again sooner.
The other end of the spectrum are too many telehealth companies that talk to you for ten minutes, prescribe the semaglutide (“base” of Ozempic and Wegovy) or tirzepatide (“base” of Mounjaro and Zepbound) take your money, then send you on your way. You might not talk to anyone else ever again, but just pay your money and get your prescription each month.
Then there are an endless variety of inbetweens, including suggesting or requiring nutrition classes, physical therapy education, membership to a gym, even psychological therapy to work through the multitude of changes and concerns that come up while taking your GLP-1. Each practitioner has their own method and thoughts around why they require one thing or four others.
Sometimes you can pick and choose, sometimes not. Sometimes insurance will pay for the extras, sometimes not. Many times there are accessibility issues at play, financially and transportation-wise.
Short Note About Racial, Ethnic, and
Socioeconomic Inequities with GLP-1s

This will be a post all on its own, but requires a mention. This issue is crazy-making for those who hunger for equality when it comes to resources, especially resources as basic as proper food, healthcare, medications, and education.
Economically, ethnic, and racially marginalized communities have been left behind, not only in the possibilities of getting the GLP-1s for their Type 2 Diabetes and/or obesity or overweight, but even in the Clinical Trials of most medications, these important meds included. Obstacles such as Medicaid and Medicare not paying for weight loss medications, transportation to and from doctor’s appointments, and food insecurity can impact diverse communities’ abilities to obtain the GLP-1s. These are merely the obvious barriers. Many nuanced roadblocks exist that must also be addressed. Everyone who needs or wants the meds should be able to access them.
I will address this in its own post soon.
Ask Your Questions in the Comments

If I have left out anything you want to know, please ask in the comments. I want to offer as much help as possible to get all the people who need and want them, their GLP-1 medications.