One of the most controversial topics from the beginning of time has been discussing a person’s weight, but especially weight loss. This has never been more challenging than now with the dawn of weight loss medications. Having been a part of this weight topic almost since my birth 63 years ago, I have participated as a speaker, blogger, writer, and victim of the discourse.
Even in this volatile time of semantics, I consider myself an Obesity Activist. For me, that is continuing to make space for people with obesity and overweight. As a midwife, I worked hard to serve women who were large and super-sized… like myself. I have collaborated with a variety of providers, including doctors, chiropractors, nurse-practitioners, and nurses to guide them in the care of people with obesity and super-obesity.

Not only have I been the super-sized care provider, I’ve also been the the really fat patient with a BMI up to 73 at times. My blog post “Fat Activist on GLP-1s: An Oxymoron?” chronicles the indignities I’ve been dealt at the hands of medical folks.

It is with those memories, that I come to you doctors, nurses, practitioners, and providers to share my personal knowledge of how to speak to people about their weight, and when and how to shift the discussion to weight loss, including the idea of going on a GLP-1 such as Zepbound or Wegovy.
Asking Permission is Crucial
It can be annoying to providers to have to ask permission of a client. I know time is of the essence and extra words take up precious seconds, but this request (or admonition, if you will) is a valuable one to build the ultimate trust with, and compliance from, your patients.
Various Ways to Begin a Non-Threatening Visit

- Leave your size, weight, racial, economic, and ethnic prejudices outside the exam room.
- Take a deep breath before you walk in the door, especially if you know there might be a difficult discussion.
- “What brings you here today?”
- “Do you have any specific issues you want to talk about?”
- “Are you concerned about anything with your health?”
- “Is this a good time to talk about your health goals?”
The Dreaded Scale

Office managers, this piece of information is for you: Please, please, PLEASE get a scale that goes over 300 pounds, and over 400, if possible. I spent years refusing to weigh at the doctor’s visits because the scale (usually a balance scale) only went up to 300 pounds and I was far above that. When I got above 400, it was even more distressing thinking no one took someone my size into consideration and I might have to go to the post office to weigh on their scale. That is what my imagination said, anyway. There certainly have to be office scales that go at least up to 400 pounds. Please buy one.
This is for the staff who does the ushering around and doing the vitals, but this is really important.
Unless you are like me, losing buckets of weight, people generally despise the scale. As a midwife, I learned early on to weigh people backwards so they did not have to look at the numbers. They are charted and factored into your diagnosis, but the patient doesn’t feel compelled to miss appointments because of having to look at their weight face to face.
You might think I am exaggerating, but I have talked to many, many people who either will not go to the doctor at all or will cancel appointments specifically because they have to weigh themselves. Allowing people to turn around backwards is a wonderful way to bring them in and still not traumatize them with the numbers.
It’s best policy to ask every patient, “Do you want to weigh frontwards or backwards?” Thin, obese, everyone. That way no one feels singled out or marginalized.
When a Health Issue Arises
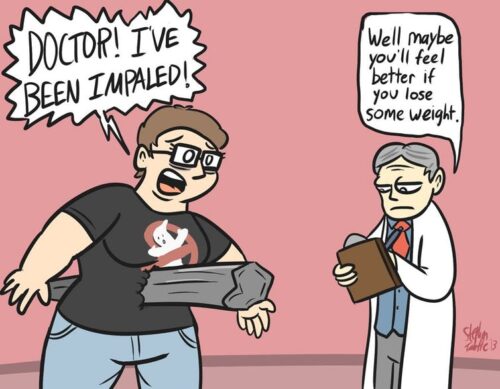
- Please do NOT just assume it is the patient’s weight causing the problem.
- Even if you are sure weight is a contributing factor, do not mention it first.
- “Hmmm… I see you have <fill in the blank>. There can be many causes of this. May I share them with you?” This way you are showing that there are choices the person can start with, the one that makes them comfortable. You are also showing that you are not going to immediately home in on their weight… the fear of every obese patient. This builds trust, often enough to open up about their weight in a few minutes.
- “Let’s talk after your lab work comes back. It will give us more information than just the exam.” If at all possible, get lab work on the patient before your office visit. If you cannot do that, a follow-up visit, longer than the initial visit would be really helpful. When you have numbers in your hands, it is hard to avoid the topic. This gives you the avenue of intervention. You are able to offer guidance and, if you feel appropriate, medication.
- “Based on what you have told me and what I see of your trend over time is that it might be time to talk about how to help your health improve. I know that weight is a tough/sensitive topic for everyone (acknowledgement of their discomfort), but I will do my best not to make this all about your weight because it is not.”
- “Have you read anything about how obesity is a disease and not a flaw in a person’s character? (Handing them a statement about that would be great.) Thinking it is would be like telling an alcoholic to just stop drinking without offering any of the many helping tools we have at our disposal now to make that happen. We always shrugged off the statistics that diet and exercise doesn’t work for 95% of people because we didn’t know what to do. Now we do!”
Your forte, providers, is the medical discussion, so I will leave that for you. Have at it!
Food Talk

These food discussions tend to get muddied by who should be talking to patients about what, how, and when to eat. I will speak in the abstract and your offices can parse out who does this part of the visit.
Asking a patient what she eats, even if she has been keeping a food diary for you, is often doctored on the low side of intake. Many, if not most, will say they eat what their skinny sister does, but in reality, that is not quite true. I don’t believe people purposefully lie. I think they/we/I really think that, but I have sat with thousands of larger people who will say that to me while I watch both of us eat 3000 calorie meals. The reality of how much we eat is painful to acknowledge. Until after my RNY Gastric Bypass in 2001 and now as I am on GLP-1s and look back at my Uber Eats and grocery bills, am I able to acknowledge I ate about 6000 calories a day. On a good day. I cried at the reality of my disease.
Reminding the person, not incessantly, but periodically, that obesity is a classified disease and the brain and body are clawing for food all the time.
You might mention Food Noise because many people have no idea others have food noise, too. “The food noise is the brain’s way to make your body think we are starving and must find food now or we will die. That’s not going to happen, but that impulse in the brain knows no logic.”
NOW Bring GLP-1s Into the Discussion

This might seem like a circuitous route to the wondrous GLP-1 and GIP/GLP-1 medications. You will find your own rhythm and path to this place. Speaking of losing food noise is a wonderful start.
“Besides weight, there are great benefits to the meds and we’re learning more every day.”
If you do give a prescription, it’s important to mention that 15% of patients do not lose weight on either semaglutide, tirzepatide, or both. That again, it is not usually their fault when they are trying hard to help it work. (I talk about the meds as a collaborative effort with their bodies.) I explain that technology has not caught up with their unique needs, but they are working hard and fast to get the right meds to the right people. Letting them know it can take three months to know if it will work helps a lot. So many want to lose 20 pounds in a week (not kidding) and if they don’t, they think it doesn’t work.
Edit Add: Please give your T2DM patients a dual diagnosis of obesity or overweight (if that fits, of course) because in this shortage, many of us on Mounjaro of Ozempic have tried to get Zepbound or Wegovy, but our insurance will not cover because we do not have the dual diagnosis. It would help us a lot if you could do that for us.
What Next?
I will write another post about topics for once the patient is on the medications. Things like baseline DEXA scans and how to start Stage II, III, IV, and V obesity patients on a movement journey that will bring them joy and continuity. Saying, “Exercise/Walk and do resistance training” isn’t appropriate or enough direction. However, I have simple ideas that will, and have, gotten people moving and strengthening.
Thank you, providers and practitioners for reading all of this. You can see my passion to make the medical experience for those with Obesity and Overweight as helpful and pleasurable as possible. I believe this is an audience that deserves special care. Too much damage has been done over the decades, some minor repair work will go a very long way.