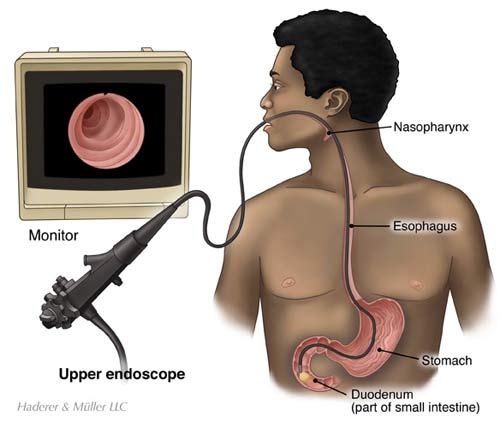
I was supposed to have a colonoscopy and endoscopy a couple of months ago, procedures that require deep sedation. I got a call a week before, asking if I was on GLP-1s. Mind you, my chart said I was on Mounjaro, but they apparently didn’t check there. When I said I was on Mounjaro, they said I needed to stop the medication a week before the procedures. I had just had my shot the day before, so that wasn’t going to happen. The nurse I was speaking to said, “Well, we can try, but if you have any gastric contents or intestinal contents, we will have to cancel the procedure and re-schedule.
This was not acceptable to me.
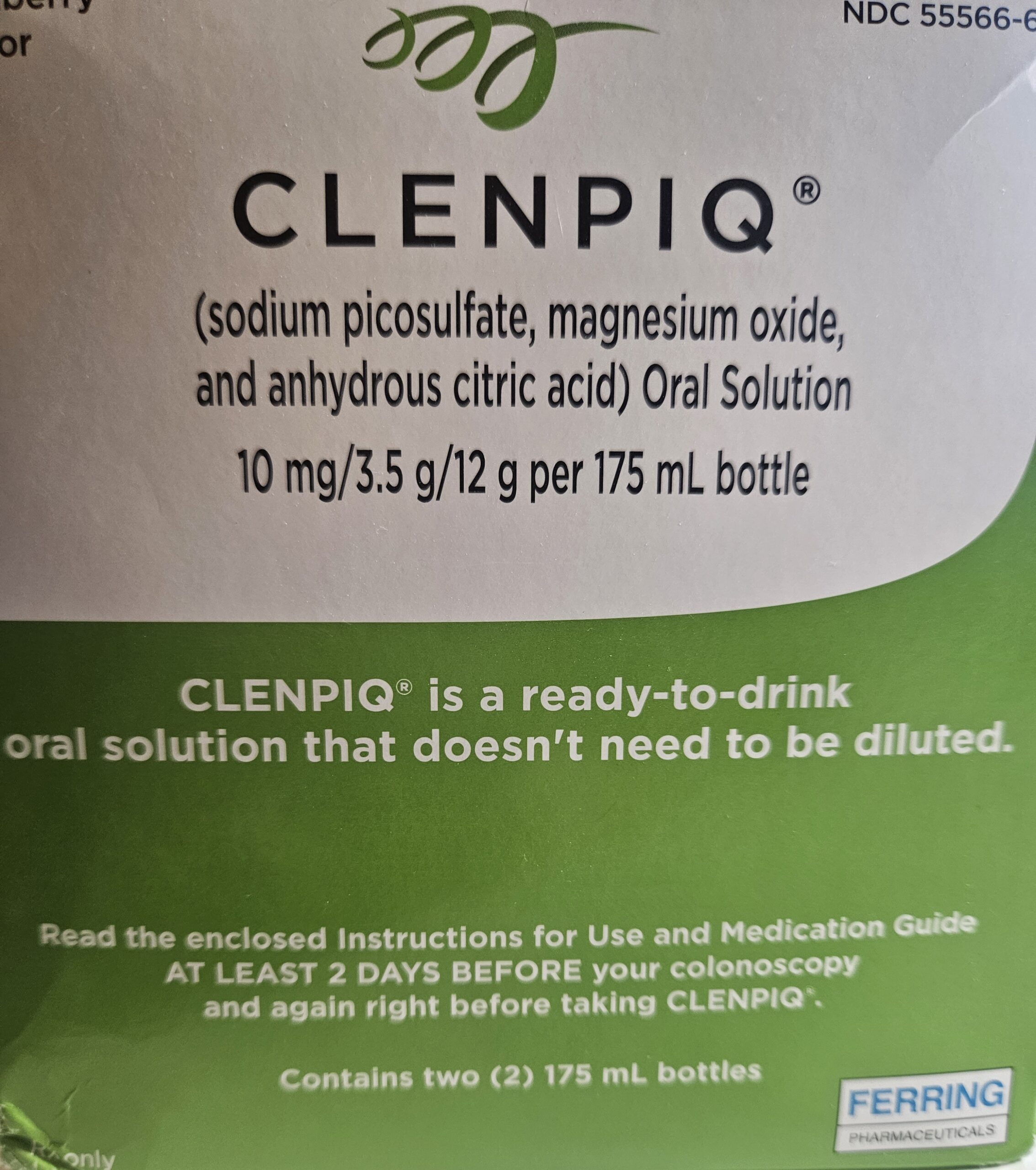
I was supposed to do the ghastly colonic prep and might possibly have to do it again? No freakin’ way. I canceled my appointment.
I’m not sure if I would be willing to stop my Mounjaro for a week or two in order to have a colonoscopy and endoscopy. As of now, I have not rescheduled.
What Does the Research Show?
It depends on who you ask or which study you read.
Stop GLP-1 RAs Two Days Before Procedures
The Journal of the Canadian Association of Gastroenterology looked at 67 articles relevant to this topic and published this February 2023 paper: Preparing for Colonoscopy in People with Diabetes: A Review with Suggestions for Clinical Practice and made recommendations reviewed by endocrinologists and gastroenterologists. This article came out in February 2023.
GLP-1 RAs are Glucagon-like peptide-1 receptor agonists, including: Dulaglutide (Trulicity), Liraglutide (Victoza/Saxenda) , Semaglutide (Ozempic/Wegovy and Rybelsus), Exenatide (Byetta), Lixisenatide (Soliqua) and Tirzepatide (Mounjaro/Zepbound).
This is their recommendation:
Recommendation: GLP-1 RAs should be stopped when the clear fluid diet begins. Once meals have resumed, GLP-1 RAs should be resumed at the normal dose and interval. If a patient takes a once-weekly injectable GLP-1 RA, the dose should be held if it is scheduled within two days before colonoscopy. If held, it should be resumed on the evening of the procedure.
And I am going to share the whole section here and bold what I will talk about after the quote.
The most common side effects of GLP-1 RAs are its effects on the GI tract (e.g., nausea, diarrhea, vomiting and delayed gastric emptying) (49). The increased risk of developing preprocedure nausea with GLP-1 RAs versus insulin leads to poorer patient experience and an increased incidence of rescheduled colonoscopy (50). Another study found that delayed gastric emptying does not appear to have an impact on the adequacy of bowel preparation, but further investigation is required as this study did not examine the effects of different classes of GLP-1RAs despite their differing effects on the GI tract (51). Furthermore, GLP-1 RA use has been linked to the development of AKI, largely due to intravascular depletion secondary to fluid loss with vomiting and diarrhea and decreased fluid intake, which can be exacerbated during colonoscopy bowel preparation (49).
Anything that says, “increased incidence of rescheduled colonoscopy” isn’t going to go over well with those of us who have to have a day’s or two’s worth of diarrhea to “prep” for the procedures.
It makes me crazy they didn’t even look at the different GLP-1s to see if there was a difference with the various peptides. Couldn’t researchers have seen that question coming?
Then we get to Acute Kidney Injury (AKI). AKI is a possibility with any of the GLP-1 medications because of the nausea, vomiting, and diarrhea. If a person vomits and/or has diarrhea so much they become dehydrated, enough to be hospitalized, then the kidneys can freak out and fail.
Most cases of AKI are caused by reduced blood flow to the kidneys, usually in someone who’s already unwell with another health condition.
This reduced blood flow could be caused by: low blood volume after bleeding, excessive vomiting or diarrhoea, or severe dehydration
Can AKI be reversed?
If AKI is treated early, most people will return to their previous kidney function. If you were healthy before AKI and you get treated right away, your kidneys could work normally or almost normally after treatment.
Back to the colonoscopy and endoscopy preparation, if someone has diarrhea and vomiting from the GLP-1 and then adds the diarrhea and vomiting inducing (and gagging) prep, it can be really dangerous AKI-wise.
Sounds fun, doesn’t it?
Stop GLP-1 RAs a Week Before Any Anesthesia

Anesthesiologists have stricter guidelines for stopping the GLP-1 RAs. From American Society of Anesthesiologists Consensus-Based Guidance on Preoperative Management of Patients (Adults and Children) on Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists. This article came out June 29, 2023
Day(s) Prior to the Procedure:
-
For patients on daily dosing consider holding GLP-1 agonists on the day of the procedure/surgery. For patients on weekly dosing consider holding GLP-1 agonists a week prior to the procedure/surgery.
-
If GLP-1 agonists prescribed for diabetes management are held for longer than the dosing schedule, consider consulting an endocrinologist for bridging the antidiabetic therapy to avoid hyperglycemia.
Day of the Procedure:
- If gastrointestinal (GI) symptoms such as severe nausea/vomiting/retching, abdominal bloating, or abdominal pain are present, consider delaying elective procedure, and discuss the concerns of potential risk of regurgitation and pulmonary aspiration with the patient.
- If the patient has no GI symptoms, but the GLP-1 agonists were not held as advised, proceed with ‘full stomach’ precautions… If the stomach is full, consider delaying the procedure or treat the patient as ‘full stomach.’ Discuss the concerns of potential risk of regurgitation and pulmonary aspiration with the patient.
- There is no evidence to suggest the optimal duration of fasting for patients on GLP-1 agonists. Therefore, until we have adequate evidence, we suggest following the current ASA fasting guidelines.
Clearly, this is much more conservative than the Canadian Association of Gastroenterology’s advice.
What if You NEED the Surgery or Colonoscopy and Endoscopy?
I am lucky in that I am not in an urgent situation where I really need the procedures. It’s just time for them. I am willing to delay them in order to keep taking my Mounjaro. But, if you have a history of Colon Cancer or are symptomatic for an illness and are getting a medical opinion to have both the procedures, talking to your doctor about what to do about your GLP-1s is going to be important. See what their recommendations are, continue researching the latest information, and proceed as you need to.
And then, of course, if you need an urgent surgery, it is the anesthesiologist’s job to watch if you have gastric contents and, if you vomit, to take care of you, helping you not inhale the contents, possibly causing pneumonia. It can happen, but is rare.
What Will You Do?
Let me know in the comments what you ended up doing. Delaying a procedure? Going ahead with it? What were the directions you were given and what was their reasoning.
I would love to hear from you.