Please Do Not Start Mega-Vitamin D Supplements
Until You Have a Blood Test
and a Care Provider Prescribes
How Much You Need to Take!
It is VERY Individual and Can Be
TOXIC
If Too Much Is Taken.

I’ve lived with extreme Vitamin D deficiency for decades because of the RNY Gastric Bypass I had in 2001. For years, I had to take 50,000 iu four times a week. I was always over 350 pounds during those supplement years.
As a comparison to my 50,000 iu four times a week, below is the chart for healthy folks’ Recommended Daily Allowance (RDA):
Children up to 12 months: 400 international units (IU)
People ages 1–70: 600 IU
People over 70: 800 IU
Pregnant or breastfeeding people: 600 IU
Toddlers, older children, and adolescents: 600 IU
Whenever I saw a new doctor, they were shocked at how much Vitamin D I was taking and still being deficient in the vitamin. 50,000 iu. four times a week is an extraordinary amount of vitamin intake.
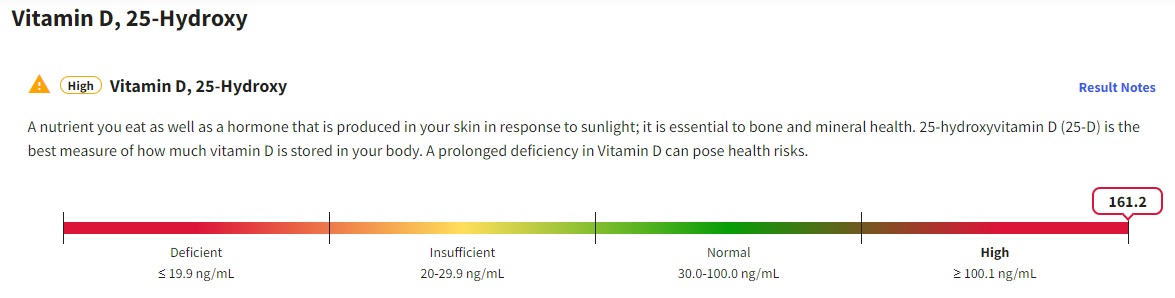
As I started losing weight, however, my D labs started climbing. I was lowered first to 50,000 iu. three times a week, then twice a week, then once a week. When my D labs kept climbing and were abnormal and, in fact, in the toxic range. three months ago, I was taken off the medication completely.
My last labs a couple of weeks ago showed my D again in the toxic range (extremely high abnormal) and the Endocrinologist called in distress the next day when she got the labs. Everything else was amazing, but the D was incredibly high. “Did you stop taking the Vitamin D like we talked about three months ago?” I told her I had and she said I might not ever have to take D again in my life. Not sure if she was kidding or not.
What Does Vitamin D Have to Do with GLP-1s?
As I looked into why my Vitamin D kept climbing despite not taking as much medication, I began to see an interesting pattern that did have a seeming connection to GLP-1s.
One of the major symptoms of a Vitamin D deficiency is gastrointestinal issues. From Irritable Bowel Syndrome (both D and C) to Inflammatory Bowel Disease.
Polycystic Ovary Syndrome (PCOS) also has a connection to Vitamin D deficiency. As does Pre-Diabetes being nudged to Diabetes with lack of Vitamin D.
And hey, we can throw hair loss and suicidal thoughts in there, too.
The last piece of the puzzle as I try to figure this out, was how does Vitamin D act in a body that has severe obesity, plain obesity, and then in someone with overweight. What I found was most intriguing.
Haylee Hannah, RD, registered dietitian and certified specialist in obesity and weight management says:
“Vitamin D deficiency is common in people with obesity, with reported prevalence rates as high as 90%. The higher risk of deficiency is thought to be related to several factors. One contributor could be less sun exposure. In addition, since vitamin D is fat-soluble, people with higher amounts of body fat will ‘sequester’ vitamin D in fat cells, leading to lower amounts circulating in the blood. Due to this, people with obesity typically need higher amounts of vitamin D to maintain adequate levels and/or to correct a deficiency.”
I also learned that where the adipose tissue (fat) is stored makes a difference. This next section discusses Visceral Adipose Tissue, or VAT. VAT is the fat we have stored around our midsection.
A long article called, “Unraveling the Connection: Visceral Adipose Tissue and Vitamin D Levels in Obesity” in the Journal Nutrients discusses the mechanisms between VAT and Vitamin D availability.
Our findings suggest that in visceral adipose tissue, vitamin D is stored, but may become trapped, leading to its reduced availability for metabolic processes. These results support the hypothesis that adipose tissue acts both as a potential reservoir and sequestration site for vitamin D.
The strong correlation between visceral adipose tissue and vitamin D levels highlights the significance of adipose tissue in influencing vitamin D levels. The storage or sequestration of vitamin D in adipose tissue may have implications for individuals with obesity or abdominal obesity, as they are more likely to have insufficient or deficient vitamin D levels. This finding aligns with previous studies that have shown an inverse relationship between abdominal obesity and vitamin D levels
My Theory About GLP-1s and Vitamin D Deficiency
With the growing knowledge of my own Vitamin D experience and what I am learning now, I’m wondering if Vitamin D deficiency can affect those of us on GLP-1s. I also have ideas of what to do with the information.
Mind you, this part is all conjecture and I am hoping studies will come out and verify or deny if those of us on GLP-1s might or might not have the tendency to have Vitamin D deficiency.
A majorly loud caveat: Correlation does not mean causation. Just because two things look like they are connected could be a complete coincidence. This goes for alllll of these thoughts I have swirling around in my head.
The first thing that comes to mind is the gastrointestinal (GI) symptoms common with GLP-1s. Why do some people have extreme symptoms and others like me have nothing but mild constipation? Do folks with more GI symptoms have lower Vitamin D levels?
Over half of patients with symptoms of gastroparesis have low vitamin D levels, which is linked to heightened nausea, vomiting, and gastric neuromuscular dysfunction.
What I wouldn’t give to get my hands on the Vitamin D labs of those suing for gastroparesis and demanding that the pharmaceutical companies add a warning about gastroparesis on the box.
Because so many women are on GLP-1s because of PCOS, does D also help heal PCOS, with or without GLP-1s?
Some literature validates that PCOS might be helped with Vitamin D supplementation.
Vitamin D deficiency might exacerbate some symptoms of PCOS. Along with PCOS treatment, taking a daily vitamin D supplement with 600 IU may help some PCOS problems such as infertility, weight gain, and anxiety.
As folks begin losing weight on the medications, does the D stored in the body become more bioavailable and the GI and PCOS symptoms abate?
Could GLP-1s alleviate chronic Vitamin D deficiency and thereby begin to heal the plethora of symptoms that come from inadequate D?
I would love to see some studies done on this topic.
New Vitamin D Protocols Might Be in the Way to
Getting Tested
The Endocrine Organization came out June 3, 2024, with new protocols regarding dosages and testing for Vitamin D levels. You can read the Press Release Endocrine Society Guideline recommends healthy adults under the age of 75 take the recommended daily allowance of vitamin D to get the whole gist of what they are saying.
The part that affects those of us on GLP-1s, however are these two paragraphs: (my emphasis)
We identified the following populations that may benefit from supplementation above the intakes recommended by the IOM (Institutes of Medicine) because of the potential to reduce specific health risks:
People with prediabetes—potential to reduce progression to diabetes.
and
We suggest against routine testing for 25-hydroxyvitamin D levels in any of the populations studied, since outcome-specific benefits based on these levels have not been identified. This includes 25-hydroxyvitamin D screening in people with dark complexion or obesity.
So even as I all but command you to get your D tested before taking any D supplements, if your care provider has read the new recommendations, you might have to gently insist on getting tested.
If you want to or need to pay cash, several labs, including LabCorp and Quest Health, allow you to order your own test. They are called customer/patient/consumer initiated tests. Prices might differ depending on where you are, but here, the LabCorp Vitamin D test is $99. The Quest Vitamin D test is $63.60. Google your closest lab and see if you can order a D lab test on your own and the price will be in there.
Finally,
I would love to know your thoughts, especially if you are a care provider. What do you think of the new protocols with regards to those of us on GLP-1s since we are on them for a wide range of symptoms that might mean our D is too low.

If they can make an at-home Covid test, why can’t they make an at home vitamin D screening? It doesn’t have to be anything elaborate, just either, it’s okay, or it’s not okay, consult your physician. I can’t remember if my vitamin D has ever been tested before, hmmm.
Agree!!!
While D seems like it is more benign than COVID, there really can be major bone consequences. You are right!