As I started my GLP-1 excursion (more than a journey, less than a whirlwind) a couple of years ago with Trulicity, I was never told about not putting the injections from the pen into the same place all the time. I’d been on insulin for over ten years by that point and I don’t remember one person ever telling me not to inject the insulin in the same area. I used both needles and pens depending on the insulin, and almost always injected in my upper belly. It was years before I learned insulin needs to be absorbed evenly allowing the blood glucoses to remain steady in the body and the abdomen is the best place to do that as I will point out in a few.
I’m going to talk about insulin first. While it might seem odd to do this, I believe it’s quite relevant to the GLP-1 topic and where to inject the medications like Mounjaro, Zepbound, Ozempic, Wegovy, and the other ‘tides medications. Everything builds on each other.

Insulin & GLP-1 Absorption
In the article “What are the best insulin injection sites?,” it’s explained:
The body absorbs insulin at different speeds from each of the sites. This information can be useful when planning insulin injections:
Abdomen: Insulin enters the bloodstream most quickly after an abdominal injection.
Upper arms: The body absorbs insulin at moderate speed but slower than an injection in the abdomen.
Thighs: Insulin enters the bloodstream less quickly than the abdomen or arms.
Buttocks: Insulin enters the bloodstream most slowly from this site.
Site of injection — It is very important to rotate injection sites (ie, avoid using the same site each time) to minimize tissue irritation or damage. When changing sites, it is important to keep in mind that insulin is absorbed at different rates in different areas of the body.
Insulin is absorbed fastest from the abdominal area, slowest from the leg and buttock, and at an intermediate rate from the arm. This may vary with the amount of fat present; areas with more fat under the skin absorb insulin more slowly. (emphasis mine)
We who are using GLP-1s are given the same injection site information, but for us, we exclude the buttocks. I wondered if our GLP-1s also absorb at the same rate as insulin in each of the areas… faster in the belly and slower in the thigh… but it turns out not to be the same.
While our GLP-1s are designed to take time, sometimes eight to ten weeks, before we have the “onset of action.” which is when we begin to feel and experience the majority of the positive effects.
This onset of action stability is the main reason people need to stay on the meds for at least three months before they even wonder if the medication is working or not.
There are different types of insulin, each type is meant to be absorbed at different rates, too. This is without the variable of location of injection. We on GLP-1s have one medication to concern ourselves with, not variables like a diabetic (both Type 1 & 2) does.
While these details are not just for Type 1 diabetics, I want to say that, in all my years on insulin as a Type 2 diabetic, I was never once counseled about these specifics. If it were not for the Internet, I would have been clueless… and was for most of my years on insulin.
Because of my early ignorance about the absorption of insulins, I think it’s crucial for those of us on GLP-1s to know what is happening with our bodies when we are injecting our medications.
Why Do We Change Injection Sites?
Lipodystrophy (the loss of fatty tissue) and Lipohypertrophy (a buildup of fatty tissue) are the two main reasons we alternate sites for our injections. This is talked about with diabetics who are on insulin more than those who have never injected themselves before, like those of us on GLP-1s. Because there are so many of us on these medications for weight loss, I thought it would be good to go over this topic.
For the GLP-1 community, lipohypertrophy is the more likely outcome of repeated injections of our meds. This can and does vary depending on individuals, but, by far, more diabetes and GLP-1 users would be at increased risk for lipohypertrophy.
Lipohypertrophy, in basic-people-speak, means that when you inject yourself in the same place, scar tissue forms. The more you inject in the same place, the more scar tissue forms. If that happens, the substance you are injecting might not be absorbed properly into your body. My theory is this might be happening with “non-responders.” I’d love to see some studies on whether this is happening or not.
Do Injection Sites Matter with GLP-1s?
Quite possibly. Someone who injects into their stomach might be absorbing the medication more quickly than if they injected into their thigh. There are many medications that, when assimilated into the body quickly, can cause more acute side effects than if they had been absorbed slower.
Yes, many are in pill form when we see them, but they can, and are, given intravenously in the hospital. If the meds are “dumped” into the IV (the IV run too quickly), it’s common for a negative reaction to occur. Here is a short list of medications that typically have negative effects/side effects when they hit the body’s system too quickly.
- Pitocin
- Insulin
- Stimulants
- Opioids
- Parkinson’s medications
- Some antibiotics (which can also cause GI symptoms if taken on an empty stomach)
- Heart medications
- Anti-anxiety meds
And back to the lipohypertrophy, because scar tissue isn’t a single mass that grows together the more of it is there is, one injection in a certain site might be super-efficient, not having gone into any scar tissue, giving great results with that week’s shot. The medication injection given into the the same site the next week might be going into scar tissue and thought of as “not working.” It might actually be because the needle went through a scarred area and the medication was unable to absorb into the body properly.
This can be the reason some injection sites work better for some people than others when giving themselves their Mounjaro, Ozempic, Zepbound, or Wegovy shots.
Why then, do the effects and side effects differ between people who inject in the same body part? Because every body is different and everyone’s metabolism mechanisms are different, too. A body part that works great for one person, not causing bad side effects, could be the exact site that gives someone else the most side effects. It can be that individual.
Asking people what worked for them is fine, but know that it might not be The Perfect Site you hope it will be. That site is great for them, but the worst site for you. Experiment if you are having side effects or not losing what your provider thinks you should/could be losing.
Remember, it is completely normal to 1) not lose a lot of weight in a week 2) to have lulls/stalls/resting time for our weight loss over many days or even weeks at a time. These two important points can occur during the entire time we are taking our GLP-1s.
Where is Our Patient Education?
Patients who use subcutaneous insulin should be examined for injection-site complications at every clinic visit and should receive counseling regarding the importance of rotating injection sites to allow sites to heal.
Has anyone’on GLP-1s had their stomach, thigh, or back of the arm examined by a healthcare provider at a follow-up appointment? If so, I have not found that person yet. Certainly not me!
Has anyone had any of this education while on their diabetes or weight loss medication? I never have. I only know this information because of my midwifery education.
Proper Way to Inject GLP-1s
So how do we avoid lipodystrophy or lipohypertrophy?
Many people will go back and forth from their left to right side of the body and inevitably choose the same places. To avoid this, many diabetes education and care specialists will recommend picking some sort of rotational pattern. Some people use letters such as “W” or “M”, others use the “planting the seed method” where you inject about a half inch away from the last injection site.
Keeping a record of your shot sites can be a valuable habit to get into.
If you have been taught to inject yourself by your provider, please follow those instructions. If you have not been told, learning how on the Internet can make you more confused than if you were just going to wing it on your own.
I am not an expert, but I encourage you to 1) ask your provider how they want you to inject 2) watch a few videos done by medical folks that show how to inject subcutaneous medications (the kind we do with GLP-1s) 3) then experiment to see what is easiest and least painful for you.
You can definitely take in information from other people on GLP-1s in support groups online, but be smart and use your judgment. If something sounds stupid or wrong, don’t do it! Otherwise, feel free to learn and the find your own method with all the information from professionals and those you are reading in social media.
I will share well-known practices of injections from my own midwifery experience (giving them), and as a patient (getting them), and taking info in from respected medical sites. I am not culling information from support groups. I will leave that up to you if you desire.
Get your supplies (alcohol wipes, syringes and vial, GLP-1 or GIP/GLP-1 pen, Sharps container out and ready, but make sure things are not within the reach of young ones or others who might want your medication that is not prescribed to them.












That’s it!
A Few Added Thoughts About Injections
I’ve seen people pinch their skin before injecting… and many nursing schools insist on it, but that isn’t typically necessary unless you are near a muscled area. If you have plenty of skin and fat like I do, no need to pinch. This pinching issue has been studied for years with diabetics with their insulin and there doesn’t seem to be a consensus. First, of course, ask your doctor, but if it helps to avoid pain when you pinch, it might not make much of a difference in bioavailability.
Try not to inject it into hanging skin. This medication needs to go into fat so it can be absorbed properly. I thought it would be easy for me to just inject into my dangling skin on my arm instead of the back of my arm. That injection was a waste because I had a freakin’ hard week of hunger. I should have known better, too! We need to make sure there is still fat under the loose skin. Don’t make the same mistake I did!
Pushing the needle (with compound GLP-1 or name brand vials) or the pen end into the injection site can be done a couple of ways equally. Caveat: If you are thin and do not have a lot of fat into which to push the needle, you do it a little bit differently. I will explain in a moment.
Mount Sinai Hospital gives information about how to use a needle and syringe if you are injecting a compounded medication or if you are in a country that uses the name brand vials. We here in the United States will also have the lower doses of Zepbound in vials soon.
-
Wash your hands.
-
With the hand that is not holding the syringe, pinch an inch (2.5 centimeters) of skin and fatty tissue (not the muscle) between your fingers.
-
Quickly insert the needle all the way into the pinched skin at a 90-degree angle (45-degree angle if there is not much fatty tissue).
-
Once the needle is all the way in, release the skin.
-
Inject all the medicine by pushing in the plunger.
-
Once the medicine is all in, pull out the needle quickly.
-
Put the needle in your sharps container.
-
Press clean gauze on the site and hold pressure for a few seconds to stop any bleeding.
-
Wash your hands when you are done.
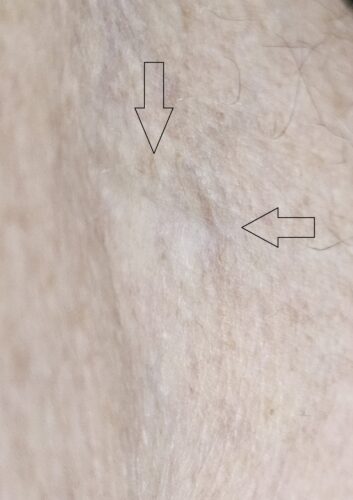
What if I Get a Lump Under My Skin After an Injection of GLP-1?
While this below speaks specifically to insulin, it is appropriate for those on diabetes or weight loss medications, too.
There are a few reasons these lumps can happen. A bump means you may have injected the insulin just under the skin instead of into fat tissue. The needle may not have gone deep enough, or you may have been pulling the needle out before the plunger reached the bottom of the syringe.
Let’s start with, if you are worried AT ALL about the lump, call your provider for advice.
Lumps right after an injection are usually short-lived and not painful. If it is painful (lump or not), you can put an icepack on it for a few minutes. If your kidneys are happy and you are someone not forbidden (like me) to take an NSAID like ibuprofen, that can help, too.
If the lump does not go away within a day or two, definitely call your provider to tell them what is going on. If it is oozing yellow or green (infection) or has a red area around where you injected and whether that red area is hot or not, do not wait the one or two days. Call your provider immediately.
What Happens if I Miss a Step?
(ie Cleaning the Top of the Vial)
Our injection experiences are medical procedures. We might not have a nurse or doctor giving us the shot, but anything that goes into our skin via a needle is something to take seriously. Our skin has bacteria on it and who knows what kind. It really is important to disinfect the skin to avoid infection.
Please do not give yourself your injection in a hurry. Please do not miss any steps that clean your hands, the vial, or your skin. Please use a new alcohol pad with the vial and another new one with your skin.
If you slack on the cleaning aspects, you can end up with an infection… minor or major.
When administering injections, doctors, nurses, and hospital staff must make sure that they are using clean/unused syringes, and that the injection site is disinfected before the injection is made. Failure to follow these simple precautions can lead to serious infections. (emphasis mine)
I’ve seen infections from injections and blood draws. They are not pretty. Taking a few seconds to clean your skin and the top of the vial can save you pain, money, and time end the end.
Clean your vials and your skin, please!
Last Words… FINALLY!
This has turned into quite the tome. I hope you made it to the end.
I care about you and your health. I know you care, too. Be good to your health. It’s why we’re taking GLP-1s in the first place, right?
Be safe and be well!