I watched “An Oprah Special: Shame, Blame and the Weight Loss Revolution.” While there are several aspects I will eventually speak about, the one outstanding issue sure to ignite great debate is having kids take GLP-1s for weight loss. As a once fat child and adolescent, then extremely fat adult, I have strong opinions about prescribing obesity meds to kids 12-17 years old.
Semaglutide Approved By FDA for Adolescents 12-17 Years Old

In December 2022, the FDA approved semaglutide, the peptide in Ozempic and Wegovy, for folks 12-17 years old. They were to be prescribed to adolescents who were in the top 5th percentile for weight. That is, they needed to be more obese than 95% of their peers.
Oh, how I wish I had had the opportunity to not be fat at 12 years old. Or 13, 14, 15, 16, or 17. My life would have been 180 degrees different.
While regular folks have thoughts about pre-teens and teens on these meds, so do a bevy of doctors, therapists, and parents.
In News Medical Life Sciences, “Experts warn of unintended consequences of using GLP-1RAs to treat childhood obesity.” (Pardon the extensive quoting. I think it’s important.)
A team of clinicians, exercise scientists, pharmaceutical scholars, ethicists and behavioral experts at the University of California, Irvine, outlined their concerns that the use of glucagon-like peptide-1 receptor agonists (GLP-1RAs) to treat childhood obesity and type 2 diabetes may have unintended and adverse consequences for children’s health.
…optimal levels of both diet and exercise increases bone mineralization during childhood, a critical period of growth and development, and this lessens their risk of osteoporosis and bone fractures later in life.
The team also pointed out the likelihood of abuse among patients with diagnosed eating disorders and children and adolescents involved in competitive sports like wrestling, martial arts, gymnastics and ballet.
The team of physicians and therapists have a six bullet point plan to keep an eye on the pediatric population that might be (and now are) going on GLP-1s.
- Studying the results on adolescents who are taking GLP-1s
- Create a Bioethics committee to study and discuss the topic.
- Create real-world data, including increasing physical fitness in schools.
- Have agencies, including the FDA, to bring in alternative ways of accurate measuring of body composition that includes food intake and output. They ask that the BMI be abandoned because it is outdated. (Don’t we ALL know that?!)
- They ask two things here: Train those on clinical trial teams to understand modern lifestyle interventions and to train pediatricians in the care of folks with childhood obesity. It specifically notes that pediatricians do not have training in this topic and need it now.
- Develop tools for teachers, coaches, parents, and children/adolescents to explain what the medications do and the risk of abuse. (I can see a “Just Say No to GLP-1 Abuse!” campaign starting up soon. Wonder who will head it this time?)
My Probable Kickstart to a Life with Obesity

I was a skinny kid up until the age of six. I wasn’t a picky eater and was too young to be out on my bike all hours of the day like I would be a few years later, so there wasn’t a real reason why I was thin. I just was.
At six years old, I got my tonsils and adenoids out liked everyone else around me. I spent one night in the hospital, not eating ice cream like they promised me. My throat hurt too much!
When I went home the next day, my mom said I began eating. Even with my hurting throat. I had steak, potatoes, and green beans. With seconds. She said they had never seen me eat so much or so fast.
I have long known it was getting my tonsils out that did this to me. Something kept me safely un-obese and it was my tonsils. When they were gone, my entire system freaked out and I began a life of uncontrolled eating.
I have written about my nurture aspects of hiding food and eating whenever there was food because we didn’t know if mom was going to have eclairs or celery sticks when we got home from school. While I believe there was a combination of nature and nurture, I can say that my experience with GLP-1s has shown me what life can be like with proper brain function; the nurture side has all but vanished.
Tonsillectomy Causing Childhood Obesity?
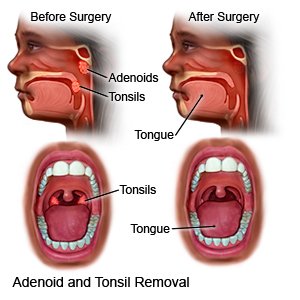
This continues to be a controversial subject. Many studies say yes, Tonsillectomy & Adenoidectomy (TA) seems to initiate childhood obesity, especially if children under six have either a tonsillectomy or TA.
Potentially worrisome weight gains following tonsillectomy occur mostly in children under the age of 6, not in older children, a study by Johns Hopkins experts in otolaryngology- head and neck surgery shows.
Sudden increases in body mass index, or BMI, have been routinely observed for months after some of the more than half-million surgeries performed annually in the United States to remove the sore and swollen tissues at the back of the throat.
They say months, but that is because many of the hundreds of studies ended a only a year after the surgery.
In “Short-Term Weight Gain after Tonsillectomy Does Not Lead to Overweight: A Systematic Review”
…data on diet composition in children after TA are conflicting, and dietary interviews in the first few months after TA could elucidate this aspect. Furthermore, adenoids and tonsils represent vital constituents of the immune system, carrying profound implications also for immunology, physiology, and the microbiome [48]. The intricate interplay between adenoids, tonsils, and various aspects of human health has been reported [48], and their removal or reduction via surgery can profoundly affect growth through different pathways.
…children who were Uw (Under weight) pre-operatively or younger than six years are reported as gaining more weight after TA than expected. Therefore, otolaryngologists and primary care providers should counsel families that increased weight gain could occur in the first 6–12 months after TA, particularly in those under six.
This review, despite what the title says, does not give, in my opinion (and I am pretty well-schooled in reading studies), overwhelming proof that TA does not encourage or cause a person to have obesity, especially as adults. In fact, the longest study reviewed went ten years past the TA date and that was just one.
Yes, I’m Cherry-Picking to Support My Belief

These paragraphs were the closest to what I know from 60+ years of asking people about their TA history.
In one analysis of 127 children six months to one year after surgery, the average body mass index of the kids increased by about 7 percent. In another analysis of 249 children, 50 to 75 percent of kids had weight gain after surgery. While most weight gain happened in the first year after surgery, scientists don’t know definitively whether it levels off after that.
The scientists wonder whether this post-surgery weight gain in young people is contributing to the nation’s obesity epidemic. That’s because tonsillectomy is the most common major operation done in childhood and more than 500,000 surgeries take place each year in the United States on kids under 15.
“This weight gain has been going on for a long time, almost four decades. Now, we need to figure out why it’s happening,” said Jeyakumar, a pediatric otolaryngologist (ear, nose, and throat specialist) at Cardinal Glennon Children’s Medical Center in St. Louis, Mo.
(all emphasis mine)
TA Takeaway

It’s hard to know what to do and when if your child has Obstructive Sleep Apnea and needs a TA. Do you wait until they are over six years old? Some doctors recommend after ten. The usual advice is:
For now, the best advice Wei (Dr. Julie Wei, a pediatric otolaryngologist and associate professor at the University of Kansas School of Medicine in Kansas City) has for parents is to “Keep a close eye on children after surgery and if you think they are gaining excessive weight, discuss this with your pediatrician.”
As someone who was a very fat child who was taken to doctors starting at 10 years old and whose mother “watched my weight” constantly, “keeping a close eye” on children after a TA isn’t going to change the compulsion for a ravenous child to eat.
What does the TA do to the body that screws it up so bad I, and many others, started as a normal-weighted children and then started stuffing ourselves two days after the TA? This is what needs to be studied.
Why?
Those of us who had our tonsils and adenoids out as young children can breathe a small (and tentative) sigh of relief that it really was not our fault for developing obesity.
This also begs the question: Did the TA cause the disease of obesity? Did it kick it in biochemically? Did it trigger a gene that would start the dominoes of obesity?
These are the questions I want answers to.
Back to GLP-1s

I turned 63 years old yesterday and weigh what I have lost: 202 pounds. I am forever grateful there is something available, albeit in a shortage at the moment, to correct whatever it is, whatever it was, that screwed my body up so badly that I could not stop eating. So many blame the person with obesity and overweight, yet we in these bodies know it is not just “Shut your mouth and move your ass.” If it was that easy, no one would be fat!
It takes a lot for me to stay calm about having had my tonsils out. The only salve for me is my Mounjaro.
It still makes me cry with relief, that it really is not my fault.
Should teens be able to use GLP-1s? Hell, yeah. Who wants to live their teen life being moo’d at? Being humiliated so badly many want to die? Let’s help these kids lead normal lives. They all deserve it.


How interesting to think/know that the tonsil removal triggered something! I wonder if my youngest’s constant ear infections all through her childhood triggered something similar. For myself, there’s nothing I can point to, except I had those constant ear infections too. There’s so many things that we just don’t know about obesity.
You are so right! Goodness, I see the research in the embryonic stage. Our grandkids and great-grandkids will look back and think of this time as the Obesity Dark Ages. Still sooooo much more to learn.